Home ANTHONY CRASTO MEDICINAL CHEMISTRY (A.M.CRASTO MEDICINAL CHEMISTRY):
'via Blog this'
Tracks information on drugs on worldwide basis by Dr Anthony Melvin Crasto, helping millions with websites, 9 million hits on google, 2.5 lakh connections worldwide, P.S. : The views expressed are my personal and in no-way suggest the views of the professional body or the company that I represent.
Saturday, 26 October 2013
Aplastic Anemia

Aplastic anemia is a rare and potentially serious blood disorder in which the body's bone marrow doesn't make enough red blood cells, white blood cells, and platelets. In many people who have aplastic anemia, the cause is unknown but may be due to one of a number of causes (eg, toxins, cancer treatment, some medicines, infections, autoimmune disorders, pregnancy). Treatments for aplastic anemia include blood transfusions, blood and marrow stem cell transplants, and medicines to stimulate bone marrow and to prevent infections. At present, there are no orphan drugs approved for aplastic anemia. For more information about aplastic anemia, visit http://www.nhlbi.nih.gov/health/health-topics/topics/aplastic/

Aplastic anemia is a syndrome of bone marrow failure characterized by peripheral pancytopenia and marrow hypoplasia, and mild macrocytosis is observed in association with stress erythropoiesis and an elevated fetal hemoglobin levels. Paul Ehrlich introduced the concept of aplastic anemia in 1888 when he studied the case of a pregnant woman who died of bone marrow failure. However, it was not until 1904 that Anatole Chauffard named this disorder aplastic anemia.
For excellent patient education resources, visit eMedicine‘s Blood and Lymphatic System Center. Also, see eMedicine’s patient education article Anemia.
Medication
The goals of pharmacotherapy in cases of aplastic anemia are to reduce morbidity, prevent complications, and eradicate malignancy.
Immunosuppressive Agents
The merits of additional immunosuppression versus the increased risk and cost should be considered. Data from a randomized prospective study indicated that an increased proportion of patients responded to the addition of CSA to ATG, but this did not translate into a long-term survival advantage.
For patients who cannot tolerate equine-based products, use of the commercially available rabbit-based ATG product (Thymoglobulin) may be considered. This product is currently approved in the United States and has been used for the treatment of aplastic anemia in Europe (although note the different dose schedule).
Cyclosporine (Sandimmune, Neoral)
Cyclic polypeptide that suppresses some humoral immunity and, to a greater extent, cell-mediated immune reactions (eg, delayed hypersensitivity, allograft rejection, experimental allergic encephalomyelitis, and graft vs host disease) for a variety of organs.
For children and adults, base the dosing on the ideal body weight. Frequent monitoring of drug levels is needed. To convert to the PO dose, use a IV-to-PO correction factor of 1:4. Dosage and duration of therapy may vary with different protocols.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
1.5-2 mg/kg IV q12h, adjust to trough level of 500-800 ng/mL in mo 1 or so; then adjust to trough level of 200 ng/mL
Pediatric
Administer as in adults.
Methylprednisolone (Medrol, Solu-Medrol)
Steroids ameliorate the delayed effects of anaphylactoid reactions and may limit biphasic anaphylaxis. In severe serum sickness (mediated by immune complexes), parenteral steroids may reduce the inflammatory effects. Hence, used with ATG to decrease the adverse effects (eg, allergic reactions, serum sickness). Also an additional immunosuppressive. High doses or long duration may be needed if serum sickness occurs with ATG. The doses and duration may vary with different protocols.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
5 mg/kg IV on days 1-8; then tapered by using PO 1 mg/kg on days 9-14; further tapering over days 15-29; stop after 1 mo except with evidence of serum sickness
Pediatric
Administer as in adults.
Lymphocyte immune globulin, equine (Atgam)
Inhibits cell-mediated immune response by altering T-cell function or eliminating antigen-reactive cells.There is little prospective randomized data to suggest a single schedule superior, but experience suggests that a short infusion is best tolerated.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
100-200 mg/kg IV total dose over variable number of days based on different protocols
Pediatric
Administer as in adults.
Cyclophosphamide (Cytoxan)
Chemically related to nitrogen mustards. As an alkylating agent, the mechanism of action of the active metabolites may involve cross-linking of DNA, which may interfere with the growth of normal and neoplastic cells. Monitor carefully; used only on an investigational basis.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
45 mg/kg/d IV for 4 d
Pediatric
Administer as in adults
Lymphocyte immune globulin, rabbit (Thymoglobulin)
May modify T-cell function and possibly eliminate antigen-reactive T lymphocytes in peripheral blood. The dose and duration of therapy vary with the investigational protocols.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
1.5 mg/kg IV qd for 7-14 d; up to 3.5 mg/kg for 5 d also used
Pediatric
Not established
Cytokines
Several preliminary studies have demonstrated that the addition of cytokines (eg, G-CSF, GM-CSF) may hasten the neutrophil recovery and that these agents may improve the response rate and survival, although long-term use may increase the risk of clonal evolution.
Sargramostim (Leukine, Prokine)
Recombinant human GM-CSF. Can activate mature granulocytes and macrophages. The dose and frequency of administration vary with the investigational protocol.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
250 mcg/m2 IV/SC with twice weekly monitoring of CBC count
Pediatric
Not established; 5 mcg/kg/d SC used in some studies
Filgrastim (Neupogen)
G-CSF that activates and stimulates the production, maturation, migration, and cytotoxicity of neutrophils.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
5 mcg/kg/d SC until ANC 5000/mm3
Pediatric
5-10 mcg/kg/d SC
Antineoplastic Agent, Antimetabolite (purine)
Antimetabolites are antineoplastic agent that inhibit cell growth and proliferation.
Fludarabine (Fludara)
Contains fludarabine phosphate, a fluorinated nucleotide analogue of the antiviral agent vidarabine, 9-b-D-arabinofuranosyladenine (ara-A) that enters the cell and is phosphorylated to form active metabolite 2-fluoro-ara-ATP, which inhibits DNA synthesis. Inhibits DNA polymerase, DNA primase, DNA ligase, and ribonucleotide reductase. This inhibits RNA function, RNA processing, and mRNA translation. Also activates apoptosis.
- Dosing
- Interactions
- Contraindications
- Precautions
Adult
30 mg/m2/dose for 4-6 d as IV infusion over 30 min-2 h
Pediatric
Administer as in adults
The theoretical basis for marrow failure includes primary defects in or damage to the stem cell or the marrow microenvironment.1,2,3 The distinction between acquired and inherited disease may present a clinical challenge, but more than 80% of cases are acquired. In acquired aplastic anemia, clinical and laboratory observations suggest that this is an autoimmune disease.
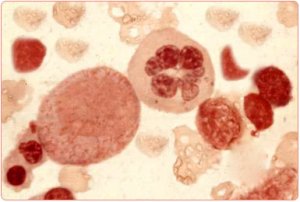
On morphologic evaluation, the bone marrow is devoid of hematopoietic elements, showing largely fat cells. Flow cytometry shows that the CD34 cell population, which contains the stem cells and the early committed progenitors, is substantially reduced.2,4 Data from in vitro colony-culture assays suggest profound functional loss of the hematopoietic progenitors, so much so that they are unresponsive even to high levels of hematopoietic growth factors.
Little evidence points to a defective microenvironment as a cause of aplastic anemia. In patients with severe aplastic anemia (SAA), stromal cells have normal function, including growth factor production. Adequate stromal function is implicit in the success of bone marrow transplantation (BMT) in aplastic anemia because the stromal elements are frequently of host origin.
The role of an immune dysfunction was suggested in 1970, when autologous recovery was documented in a patient with aplastic anemia in whom engrafting failed after BMT. Mathe proposed that the immunosuppressive regimen used for conditioning promoted the return of normal marrow function. Since then, numerous studies have shown that, in approximately 70% of patients with acquired aplastic anemia, immunosuppressive therapy improves marrow function.3,5,6,7,8 Immunity is genetically regulated (by immune response genes), and it is also influenced by environment (eg, nutrition, aging, previous exposure).9,10 Although the inciting antigens that breach immune tolerance with subsequent autoimmunity are unknown, human leukocyte antigen (HLA)-DR2 is overrepresented among European and United States patients with aplastic anemia, suggesting a role for antigen recognition, and its presence is predictive of a better response to cyclosporine.
Suppression of hematopoiesis is likely mediated by an expanded population of the following cytotoxic T lymphocytes (CTLs): CD8 and HLA-DR+, which are detectable in both the blood and bone marrow of patients with aplastic anemia. These cells produce inhibitory cytokines, such as gamma-interferon and tumor necrosis factor, which can suppress progenitor cell growth. Polymorphisms in these cytokine genes, associated with an increased immune response, are more prevalent in patients with aplastic anemia. These cytokines suppress hematopoiesis by affecting the mitotic cycle and cell killing by inducing Fas-mediated apoptosis. In addition, these cytokines induce nitric oxide synthase and nitric oxide production by marrow cells, which contributes to immune-mediated cytotoxicity and the elimination of hematopoietic cells.
Constitutive expression of Tbet, a transcriptional regulator that is critical to Th1 polarization, occurs in a majority of aplastic anemia patients.5 Perforin is a cytolytic protein expressed mainly in activated cytotoxic lymphocytes and natural-killer cells. Mutations in perforin gene are responsible for some cases of familial hemophagocytosis11 ; mutations in SAP, a gene encoding for a small modulator protein that inhibits undefined-interferon production, underlie X-linked lymphoproliferation, a fatal illness associated with an aberrant immune response to herpesviruses and aplastic anemia. Perforin and SAP protein levels are markedly diminished in a majority of acquired aplastic anemia cases.
Friday, 25 October 2013
Subscribe to:
Comments (Atom)