Functionalities can be added to nanomaterials by interfacing them with biological molecules or structures. The size of nanomaterials is similar to that of most biological molecules and structures; therefore, nanomaterials can be useful for both in vivo and in vitro biomedical research and applications. Thus far, the integration of nanomaterials with biology has led to the development of diagnostic devices, contrast agents, analytical tools, physical therapy applications, and drug delivery vehicles.
Nanomedicine is a large industry, with nanomedicine sales reaching $6.8 billion in 2004, and with over 200 companies and 38 products worldwide, a minimum of $3.8 billion in nanotechnology R&D is being invested every year.
[5] In April 2006, the journal
Nature Materialsestimated that 130 nanotech-based drugs and delivery systems were being developed worldwide.
[6] As the nanomedicine industry continues to grow, it is expected to have a significant impact on the economy.
Drug delivery
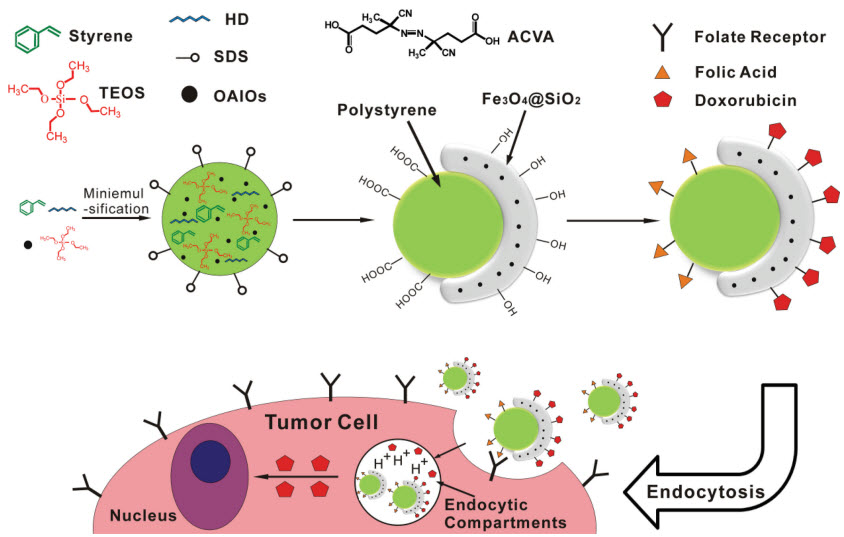
Nanotechnology has provided the possibility of delivering drugs to specific cells using nanoparticles.
The overall drug consumption and side-effects may be lowered significantly by depositing the active agent in the morbid region only and in no higher dose than needed. Targeted drug delivery is intended to reduce the side effects of drugs with concomitant decreases in consumption and treatment expenses.
Drug delivery focuses on maximizing
bioavailability both at specific places in the body and over a period of time. This can potentially be achieved by molecular targeting by nanoengineered devices.
[7][8] More than $65 billion are wasted each year due to poor bioavailability. A benefit of using nanoscale for medical technologies is that smaller devices are less invasive and can possibly be implanted inside the body, plus biochemical reaction times are much shorter. These devices are faster and more sensitive than typical drug delivery.
[9] The efficacy of drug delivery through nanomedicine is largely based upon: a) efficient encapsulation of the drugs, b) successful delivery of drug to the targeted region of the body, and c) successful release of the drug.

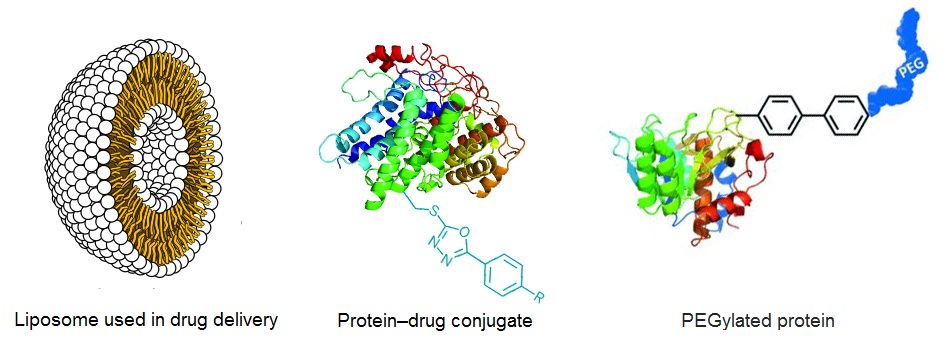
Drug delivery systems, lipid-
[10] or polymer-based nanoparticles,
[11] can be designed to improve the
pharmacokinetics and
biodistribution of the drug.
[12][13][14] However, the pharmacokinetics and pharmacodynamics of nanomedicine is highly variable among different patients.
[15]When designed to avoid the body’s defence mechanisms,
[16] nanoparticles have beneficial properties that can be used to improve drug delivery. Complex drug delivery mechanisms are being developed, including the ability to get drugs through cell membranes and into cell
cytoplasm. Triggered response is one way for drug molecules to be used more efficiently. Drugs are placed in the body and only activate on encountering a particular signal. For example, a drug with poor solubility will be replaced by a drug delivery system where both hydrophilic and hydrophobic environments exist, improving the solubility.
[17] Drug delivery systems may also be able to prevent tissue damage through regulated drug release; reduce drug clearance rates; or lower the volume of distribution and reduce the effect on non-target tissue. However, the biodistribution of these nanoparticles is still imperfect due to the complex host’s reactions to nano- and microsized materials
[16] and the difficulty in targeting specific organs in the body. Nevertheless, a lot of work is still ongoing to optimize and better understand the potential and limitations of nanoparticulate systems. While advancement of research proves that targeting and distribution can be augmented by nanoparticles, the dangers of nanotoxicity become an important next step in further understanding of their medical uses.
[18]

Types of systems used
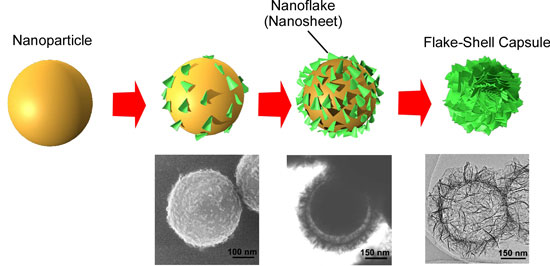
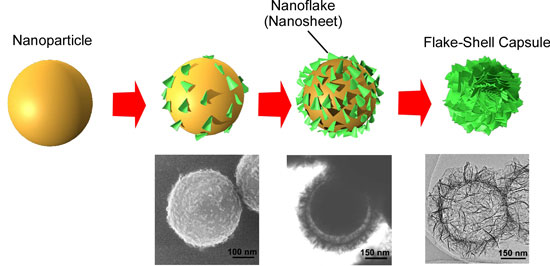
Two forms of nanomedicine that have already been tested in mice and are awaiting human trials that will be using gold
nanoshells to help diagnose and treat cancer,
[23] and using
liposomes as
vaccine adjuvants and as vehicles for drug transport.
[24][25] Similarly, drug detoxification is also another application for nanomedicine which has shown promising results in rats.
[26] Advances in Lipid nanotechnology was also instrumental in engineering medical nanodevices and novel drug delivery systems as well as in developing sensing applications.
[27] Another example can be found in
dendrimers and nanoporous materials. Another example is to use block co-polymers, which form
micellesfor drug encapsulation.
[11]
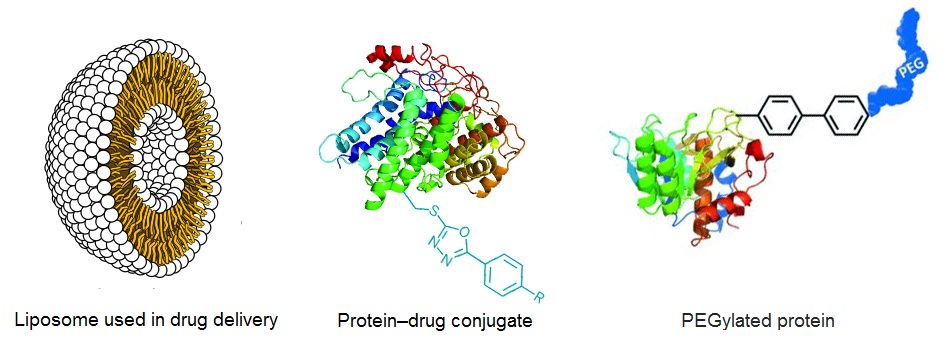
Polymeric nano-particles are a competing technology to lipidic (based mainly on
Phospholipids) nano-particles. There is an additional risk of toxicity associated with polymers not widely studied or understood. The major advantages of polymers is stability, lower cost and predictable characterisation. However, in the patient’s body this very stability (slow degradation) is a negative factor. Phospholipids on the other hand are membrane lipids (already present in the body and surrounding each cell), have a GRAS (Generally Recognised As Safe) status from FDA and are derived from natural sources without any complex chemistry involved. They are not metabolised but rather absorbed by the body and the degradation products are themselves nutrients (fats or micronutrients).
Protein and peptides exert multiple biological actions in the human body and they have been identified as showing great promise for treatment of various diseases and disorders. These macromolecules are called
biopharmaceuticals. Targeted and/or controlled delivery of these biopharmaceuticals using
nanomaterials like
nanoparticles and
Dendrimers is an emerging field called nanobiopharmaceutics, and these products are called nanobiopharmaceuticals.
Another highly efficient system for
microRNA delivery for example are
nanoparticles formed by the self-assembly of two different microRNAs deregulated in cancer.
[28]
Another vision is based on small electromechanical systems;
nanoelectromechanical systems are being investigated for the active release of drugs. Some potentially important applications include cancer treatment with iron nanoparticles or gold shells.Nanotechnology is also opening up new opportunities in implantable delivery systems, which are often preferable to the use of injectable drugs, because the latter frequently display first-order kinetics (the blood concentration goes up rapidly, but drops exponentially over time). This rapid rise may cause difficulties with toxicity, and drug efficacy can diminish as the drug concentration falls below the targeted range.
Applications
Some nanotechnology-based drugs that are commercially available or in human clinical trials include:
- Abraxane, approved by the U.S. Food and Drug Administration (FDA) to treat breast cancer,[29] non-small- cell lung cancer (NSCLC)[30]and pancreatic cancer,[31] is the nanoparticle albumin bound paclitaxel.
- Doxil was originally approved by the FDA for the use on HIV-related Kaposi’s sarcoma. It is now being used to also treat ovarian cancer and multiple myeloma. The drug is encased in liposomes, which helps to extend the life of the drug that is being distributed. Liposomes are self-assembling, spherical, closed colloidal structures that are composed of lipid bilayers that surround an aqueous space. The liposomes also help to increase the functionality and it helps to decrease the damage that the drug does to the heart muscles specifically.[32]
- Onivyde, liposome encapsulated irinotecan to treat metastatic pancreatic cancer, was approved by FDA in October 2015.[33]
- C-dots (Cornell dots) are the smallest silica-based nanoparticles with the size <10 nm. The particles are infused with organic dye which will light up with fluorescence. Clinical trial is underway since 2011 to use the C-dots as diagnostic tool to assist surgeons to identify the location of tumor cells.[34]
- An early phase clinical trial using the platform of ‘Minicell’ nanoparticle for drug delivery have been tested on patients with advanced and untreatable cancer. Built from the membranes of mutant bacteria, the minicells were loaded with paclitaxel and coated withcetuximab, antibodies that bind the epidermal growth factor receptor (EGFR) which is often overexpressed in a number of cancers, as a ‘homing’ device to the tumor cells. The tumor cells recognize the bacteria from which the minicells have been derived, regard it as invading microorganism and engulf it. Once inside, the payload of anti-cancer drug kills the tumor cells. Measured at 400 nanometers, the minicell is bigger than synthetic particles developed for drug delivery. The researchers indicated that this larger size gives the minicells a better profile in side-effects because the minicells will preferentially leak out of the porous blood vessels around the tumor cells and do not reach the liver, digestive system and skin. This Phase 1 clinical trial demonstrated that this treatment is well tolerated by the patients. As a platform technology, the minicell drug delivery system can be used to treat a number of different cancers with different anti-cancer drugs with the benefit of lower dose and less side-effects.[35][36]
- In 2014, a Phase 3 clinical trial for treating inflammation and pain after cataract surgery, and a Phase 2 trial for treating dry eye disease were initiated using nanoparticleloteprednol etabonate.[37] In 2015, the product, KPI-121 was found to produce statistically significant positive results for the post-surgery treatment.[38]

Cancer
Nanoparticles have high surface area to volume ratio. This allows for many functional groups to be attached to a nanoparticle, which can seek out and bind to certain
tumor cells. Additionally, the small size of nanoparticles (10 to 100 nanometers), allows them to preferentially accumulate at tumor sites (because tumors lack an effective lymphatic drainage system).
[43] Limitations to conventional cancer chemotherapy include drug resistance, lack of selectivity, and lack of solubility. Nanoparticles have the potential to overcome these problems.
[44]

In
photodynamic therapy, a particle is placed within the body and is illuminated with light from the outside. The light gets absorbed by the particle and if the particle is metal, energy from the light will heat the particle and surrounding tissue. Light may also be used to produce high energy oxygen molecules which will chemically react with and destroy most organic molecules that are next to them (like tumors). This therapy is appealing for many reasons. It does not leave a “toxic trail” of reactive molecules throughout the body (chemotherapy) because it is directed where only the light is shined and the particles exist. Photodynamic therapy has potential for a noninvasive procedure for dealing with diseases, growth and tumors.
Kanzius RF therapy is one example of such therapy (nanoparticle hyperthermia) . Also,
gold nanoparticleshave the potential to join numerous therapeutic functions into a single platform, by targeting specific tumor cells, tissues and organs.
[45][46]

Visualization
In vivo imaging is another area where tools and devices are being developed. Using nanoparticle
contrast agents, images such as ultrasound and MRI have a favorable distribution and improved contrast. This might be accomplished by self assembled biocompatible nanodevices that will detect, evaluate, treat and report to the clinical doctor automatically.
[citation needed]
The small size of nanoparticles endows them with properties that can be very useful in
oncology, particularly in imaging. Quantum dots (nanoparticles with quantum confinement properties, such as size-tunable light emission), when used in conjunction with MRI (magnetic resonance imaging), can produce exceptional images of tumor sites.
Nanoparticles of
cadmium selenide(
quantum dots) glow when exposed to ultraviolet light. When injected, they seep into cancer
tumors. The surgeon can see the glowing tumor, and use it as a guide for more accurate tumor removal.These nanoparticles are much brighter than organic dyes and only need one light source for excitation. This means that the use of fluorescent quantum dots could produce a higher contrast image and at a lower cost than today’s organic dyes used as
contrast media. The downside, however, is that quantum dots are usually made of quite toxic elements.
Tracking movement can help determine how well drugs are being distributed or how substances are metabolized. It is difficult to track a small group of cells throughout the body, so scientists used to dye the cells. These dyes needed to be excited by light of a certain wavelength in order for them to light up. While different color dyes absorb different frequencies of light, there was a need for as many light sources as cells. A way around this problem is with luminescent tags. These tags are
quantum dots attached to proteins that penetrate cell membranes. The dots can be random in size, can be made of bio-inert material, and they demonstrate the nanoscale property that color is size-dependent. As a result, sizes are selected so that the frequency of light used to make a group of quantum dots fluoresce is an even multiple of the frequency required to make another group incandesce. Then both groups can be lit with a single light source. They have also found a way to insert
nanoparticles[47] into the affected parts of the body so that those parts of the body will glow showing the tumor growth or shrinkage or also organ trouble.
[48]
Sensing
Nanotechnology-on-a-chip is one more dimension of
lab-on-a-chip technology. Magnetic nanoparticles, bound to a suitable antibody, are used to label specific molecules, structures or microorganisms. Gold nanoparticles tagged with short segments of
DNA can be used for detection of genetic sequence in a sample. Multicolor optical coding for biological assays has been achieved by embedding different-sized
quantum dots into polymeric microbeads. Nanopore technology for analysis of nucleic acids converts strings of nucleotides directly into electronic signatures.
[citation needed]
Sensor test chips containing thousands of nanowires, able to detect proteins and other biomarkers left behind by cancer cells, could enable the detection and diagnosis of cancer in the early stages from a few drops of a patient’s blood.
[49] Nanotechnology is helping to advance the use of
arthroscopes, which are pencil-sized devices that are used in surgeries with lights and cameras so surgeons can do the surgeries with smaller incisions. The smaller the incisions the faster the healing time which is better for the patients. It is also helping to find a way to make an arthroscope smaller than a strand of hair.
[50]
Blood purification

The small size (< 100 nm) and large surface area of functionalized nanomagnets leads to advantageous properties compared to
hemoperfusion, which is a clinically used technique for the purification of blood and is based on surface
adsorption. These advantages are high loading and accessibility of the binding agents, high selectivity towards the target compound, fast diffusion, small hydrodynamic resistance, and low dosage.
[58]
This approach offers new therapeutic possibilities for the treatment of systemic infections such as
sepsis by directly removing the pathogen. It can also be used to selectively remove
cytokines or
endotoxins[54] or for the dialysis of compounds which are not accessible by traditional dialysis methods. However the technology is still in a preclinical phase and first clinical trials are not expected before 2017.
[59]
Tissue engineering
Nanotechnology may be used as part of
tissue engineering to help reproduce or repair damaged tissue using suitable nanomaterial-based scaffolds and growth factors. Tissue engineering if successful may replace conventional treatments like organ transplants or artificial implants. Nanoparticles such as graphene, carbon nanotubes, molybdenum disulfide and tungsten disulfide are being used as reinforcing agents to fabricate mechanically strong biodegradable polymeric nanocomposites for bone tissue engineering applications. The addition of these nanoparticles in the polymer matrix at low concentrations (~0.2 weight %) leads to significant improvements in the compressive and flexural mechanical properties of polymeric nanocomposites.
[60][61] Potentially, these nanocomposites may be used as a novel, mechanically strong, light weight composite as bone implants.
For example, a flesh welder was demonstrated to fuse two pieces of chicken meat into a single piece using a suspension of gold-coated
nanoshells activated by an infrared laser. This could be used to weld arteries during surgery.
[62] Another example is
nanonephrology, the use of nanomedicine on the kidney.
Medical devices
Neuro-electronic interfacing is a visionary goal dealing with the construction of nanodevices that will permit computers to be joined and linked to the nervous system. This idea requires the building of a molecular structure that will permit control and detection of nerve impulses by an external computer. A refuelable strategy implies energy is refilled continuously or periodically with external sonic, chemical, tethered, magnetic, or biological electrical sources, while a nonrefuelable strategy implies that all power is drawn from internal energy storage which would stop when all energy is drained. A nanoscale
enzymatic biofuel cell for self-powered nanodevices have been developed that uses glucose from biofluids including human
blood and watermelons.
[63] One limitation to this innovation is the fact that electrical interference or leakage or overheating from power consumption is possible. The wiring of the structure is extremely difficult because they must be positioned precisely in the nervous system. The structures that will provide the interface must also be compatible with the body’s immune system.
[64]

Molecular nanotechnology is a
speculative subfield of nanotechnology regarding the possibility of engineering
molecular assemblers, machines which could re-order matter at a molecular or atomic scale. Nanomedicine would make use of these
nanorobots, introduced into the body, to repair or detect damages and infections. Molecular nanotechnology is highly theoretical, seeking to anticipate what inventions nanotechnology might yield and to propose an agenda for future inquiry. The proposed elements of molecular nanotechnology, such as molecular assemblers and
nanorobots are far beyond current capabilities.
[1][64][65][66] Future advances in nanomedicine could give rise to
life extensionthrough the repair of many processes thought to be responsible for aging.
K. Eric Drexler, one of the founders of nanotechnology, postulated cell repair machines, including ones operating within cells and utilizing as yet hypothetical
molecular machines, in his 1986 book
Engines of Creation.
Raymond Kurzweil, a
futurist and
transhumanist, stated in his book
The Singularity Is Near that he believes that advanced medical
nanorobotics could completely remedy the effects of aging by 2030.
[67] According to
Richard Feynman, it was his former graduate student and collaborator
Albert Hibbs who originally suggested to him (circa 1959) the idea of a
medical use for Feynman’s theoretical micromachines (see
nanotechnology). Hibbs suggested that certain repair machines might one day be reduced in size to the point that it would, in theory, be possible to (as Feynman put it) “
swallow the doctor“. The idea was incorporated into Feynman’s 1959 essay
There’s Plenty of Room at the Bottom.[68]

References
- Nanomedicine, Volume I: Basic Capabilities, by Robert A. Freitas Jr. 1999, ISBN 1-57059-645-X
- Wagner V; Dullaart A; Bock AK; Zweck A. (2006). “The emerging nanomedicine landscape”. Nat. Biotechnol. 24 (10): 1211–1217.doi:10.1038/nbt1006-1211.PMID 17033654.
- Freitas RA Jr. (2005). “What is Nanomedicine?” (PDF). Nanomedicine: Nanotechnology, Biology and Medicine 1 (1): 2–9.doi:10.1016/j.nano.2004.11.003.PMID 17292052.
- Nanotechnology in Medicine and the Biosciences, by Coombs RRH, Robinson DW. 1996, ISBN 2-88449-080-9
- Nanotechnology: A Gentle Introduction to the Next Big Idea, by MA Ratner, D Ratner. 2002, ISBN 0-13-101400-5
- Editorial. (2006). “Nanomedicine: A matter of rhetoric?”. Nat Materials. 5 (4): 243.Bibcode:2006NatMa…5..243..doi:10.1038/nmat1625. PMID 16582920.
- LaVan DA; McGuire T; Langer R. (2003). “Small-scale systems for in vivo drug delivery”. Nat. Biotechnol. 21 (10): 1184–1191.doi:10.1038/nbt876.PMID 14520404.
- Cavalcanti A; Shirinzadeh B; Freitas RA Jr.; Hogg T. (2008). “Nanorobot architecture for medical target identification”. Nanotechnology19 (1): 015103(15pp).Bibcode:2008Nanot..19a5103C. doi:10.1088/0957-4484/19/01/015103.
- Boisseau, P.; Loubaton, B. (2011). “Nanomedicine, nanotechnology in medicine”.Comptes Rendus Physique 12 (7): 620–636.doi:10.1016/j.crhy.2011.06.001.
- Rao, Shasha; Tan, Angel; Thomas, Nicky; Prestidge, Clive. “Perspective and potential of oral lipid-based delivery to optimize pharmacological therapies against cardiovascular diseases”. Journal of Controlled Release 193: 174–187.doi:10.1016/j.jconrel.2014.05.013.
- University of Waterloo, Nanotechnology in Targeted Cancer Therapy,http://www.youtube.com/watch?v=RBjWwlnq3cA 15 January 2010
- Allen TM; Cullis PR (2004). “Drug Delivery Systems: Entering the Mainstream”. Science303 (5665): 1818–1822. Bibcode:2004Sci…303.1818A. doi:10.1126/science.1095833.PMID 15031496.
- Walsh MD; Hanna SK; Sen J; Rawal S; Cabral CB; Yurkovetskiy AV; Fram RJ; Lowinger TB; et al. (2012). “Pharmacokinetics and antitumor efficacy of XMT-1001, a novel, polymeric topoisomerase I inhibitor, in mice bearing HT-29 human colon carcinoma xenografts”. Clin. Cancer Res. 18 (9): 2591–602. doi:10.1158/1078-0432.CCR-11-1554.PMID 22392910.
- Chu KS; Hasan W; Rawal S; Walsh MD; Enlow EM; Luft JC; Bridges AS; Kuijer JL; et al. (Jul 2013). “Plasma, tumor and tissue pharmacokinetics of Docetaxel delivered via nanoparticles of different sizes and shapes in mice bearing SKOV-3 human ovarian carcinoma xenograft”. Nanomedicine 9 (5): 686–93. doi:10.1016/j.nano.2012.11.008.PMID 23219874.
- Caron WP; Song G; Kumar P; Rawal S; Zamboni WC (2012). “Interpatient pharmacokinetic and pharmacodynamic variability of carrier-mediated anticancer agents”.Clin. Pharmacol. Ther. 91 (5): 802–12. doi:10.1038/clpt.2012.12. PMID 22472987.
- Bertrand N; Leroux JC (2011). “The journey of a drug carrier in the body: an anatomo-physiological perspective”. Journal of Controlled Release 161 (2): 152–63.doi:10.1016/j.jconrel.2011.09.098. PMID 22001607.
- Nagy ZK, Zsombor K.; Balogh A; Vajna B; Farkas A; Patyi G; Kramarics A; Marosi G (2011). “Comparison of Electrospun and Extruded Soluplus-Based Solid Dosage Forms of Improved Dissolution”. Journal of Pharmaceutical Sciences 101 (1): n/a.doi:10.1002/jps.22731. PMID 21918982.
- Minchin, Rod (2008). “Sizing up targets with nanoparticles”. Nature Nanotechnology 3(1): 12–13. Bibcode:2008NatNa…3…12M.doi:10.1038/nnano.2007.433.PMID 18654442.
- Banoee, M.; Seif, S.; Nazari, Z. E.; Jafari-Fesharaki, P.; Shahverdi, H. R.; Moballegh, A.; Moghaddam, K. M.; Shahverdi, A. R. (2010). “ZnO nanoparticles enhanced antibacterial activity of ciprofloxacin against Staphylococcus aureus and Escherichia coli”. J Biomed Mater Res B Appl Biomater 93 (2): 557–61. doi:10.1002/jbm.b.31615.PMID 20225250.
- Seil JT; Webster TJ (2012). “Antimicrobial applications of nanotechnology: methods and literature”. Int J Nanomedicine 7: 2767–81.doi:10.2147/IJN.S24805. PMID 22745541.
- Borzabadi-Farahani A; Borzabadi E; Lynch E. (2013). “Nanoparticles in orthodontics, a review of antimicrobial and anti-caries applications”. Acta Odontol Scand 72 (6): 413–417.doi:10.3109/00016357.2013.859728. PMID 24325608.
- Conde, J.; de la Fuente, JM; Baptista, PV. “Nanomaterials for reversion of multidrug resistance in cancer: a new hope for an old idea?.” Front. Pharmacol.2013. Vol 4 No 134.
- Sanjeev Soni, Himanshu Tyagi, Robert A. Taylor, Amod Kumar, Role of optical coefficients and healthy tissue-sparing characteristics in gold nanorod-assisted thermal therapy, International Journal of Hyperthermia, 2013, Vol. 29, No. 1 , Pages 87-97
- Jump up^ Nanospectra Biosciences, Inc. – Publications (http://www.nanospectra.com/clinicians/spublications.html)
- Mozafari, M.R. (ed), (2006) Nanocarrier Technologies: Frontiers of Nanotherapy (Chapters 1 and 2) pages 10–11, 25–34
- Bertrand N; Bouvet C; Moreau P & Leroux JC (2010). “Transmembrane pH-Gradient Liposomes To Treat Cardiovascular Drug Intoxication”. ACS Nano 4 (12): 7552–7558.doi:10.1021/nn101924a. PMID 21067150.
- Mashaghi S.; Jadidi T.; Koenderink G.; Mashaghi A. (2013). “Lipid Nanotechnology”.Int. J. Mol. Sci. 2013 (14): 4242–4282.doi:10.3390/ijms14024242. PMID 23429269.
- Conde, J; Oliva, N; Atilano, M; Song, HS; Artzi, N (2015). “Self-assembled RNA-triple-helix hydrogel scaffold for microRNA modulation in the tumour microenvironment”. Nat Mater. doi:10.1038/nmat4497.
- FDA (October 2012). “Highlights of Prescribing Information, Abraxane for Injectable Suspension” (PDF).
- “Paclitaxel (Abraxane)”. U.S. Food and Drug Administration. 11 October 2012. Retrieved 10 December 2012.
- FDA Press Announcements (6 September 2013). “FDA approves Abraxane for late-stage pancreatic cancer”. FDA.
- Martis, Elvis A.; Badve, Rewa R.; Degwekar, Mukta D. (January 2012). “Nanotechnology based devices and applications in medicine: An overview”. Chronicles of Young Scientists 3(1): 68–73. doi:10.4103/2229-5186.94320.
- Jump up^ News Release (22 October 2015). “FDA approves new treatment for advanced pancreatic cancer”. FDA.
- Gibney, Michael (18 April 2013). “Cornell nanosized ‘dots’ for diagnostics may now deliver drugs”. fiercedrugdelivery.com. Retrieved17 June 2013.
- Elvidge, Suzanne (11 November 2012). “Bacterial ‘minicells’ deliver cancer drugs straight to the target”. fiercedrugdelivery.com. Retrieved 10 December 2012.
- “First trial in humans of ‘minicells’: a completely new way of delivering anti-cancer drugs”. fiercedrugdelivery.com. 12 November 2012. Retrieved 10 December 2012.
- Press Release (19 June 2014). “Kala Pharmaceuticals Initiates Phase3 Clinical Trial for Treatment of Post-Surgical Ocular Inflammation and Phase 2 Clinical Trial in Dry Eye Disease” (PDF). Kala Pharmaceuticals.
- Press Release (1 April 2015). “Kala Pharmaceuticals Announces Positive Results from Phase 3 Trial of KPI-121 in Cataract Surgery”(PDF). Kala Pharmaceuticals.
- Wang AZ, Langer R, Farokhzad OC (2012). “Nanoparticle delivery of cancer drugs”.Annu. Rev. Med. 63: 185–98.doi:10.1146/annurev-med-040210-162544.PMID 21888516.
- Jump up^ Pérez-Herrero E, Fernández-Medarde A (2015). “Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy”. Eur J Pharm Biopharm 93: 52–79.doi:10.1016/j.ejpb.2015.03.018. PMID 25813885.
- Nguyen-Ngoc T, Raymond E (2015). “Reinvention of chemotherapy: drug conjugates and nanoparticles”. Curr Opin Oncol 27: 232–42. doi:10.1097/CCO.0000000000000183.PMID 25783982.
- Jump up^ Ghaz-Jahanian MA, Abbaspour-Aghdam F, Anarjan N, Berenjian A, Jafarizadeh-Malmiri H (2015). “Application of chitosan-based nanocarriers in tumor-targeted drug delivery”. Mol. Biotechnol. 57 (3): 201–18. doi:10.1007/s12033-014-9816-3.PMID 25385004.
- Jump up^ Nie, Shuming; Yun Xing; Gloria J. Kim & Jonathan W. Simmons (2007). “Nanotechnology Applications in Cancer”. Annual Review of Biomedical Engineering 9 (1): 257–88.doi:10.1146/annurev.bioeng.9.060906.152025. PMID 17439359.
- Jump up^ Chidambaram, M.; Manavalan, R.; Kathiresan, K. (2011). “Nanotherapeutics to overcome conventional cancer chemotherapy limitations”. Journal of pharmacy & pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques 14 (1): 67–77. PMID 21501554.
- Jump up^ Loo C; Lin A; Hirsch L; Lee MH; Barton J; Halas N; West J; Drezek R. (2004).“Nanoshell-enabled photonics-based imaging and therapy of cancer”. Technol Cancer Res Treat 3 (1): 33–40. doi:10.1177/153303460400300104. PMID 14750891.
- Jump up^ Conde J, Tian F, Hernández Y, Bao C, Cui D, Janssen KP, Ibarra MR, Baptista PV, Stoeger T, de la Fuente JM. In vivo tumor targeting via nanoparticle-mediated therapeutic siRNA coupled to inflammatory response in lung cancer mouse models.Biomaterials. 2013;34(31):7744-53. doi:10.1016/j.biomaterials.2013.06.041
- Jump up^ Yasitha L Hewakuruppu et al., Plasmonic ” pump – probe ” method to study semi-transparent nanofluids, Applied Optics, 52(24) 6041-6050.
- Coffey, Rebecca (August 2010). “20 Things You Didn’t Know About Nanotechnology”.Discover 31 (6): 96.
- Zheng G; Patolsky F; Cui Y; Wang WU; Lieber CM (2005). “Multiplexed electrical detection of cancer markers with nanowire sensor arrays”. Nat. Biotechnol. 23 (10): 1294–1301. doi:10.1038/nbt1138. PMID 16170313.
- Hall, J. Storrs (2005). Nanofuture : what’s next for nanotechnology. Amherst, NY: Prometheus Books. ISBN 978-1591022879.
- Herrmann, I. K. et al. Nanomagnet-based removal of lead and digoxin from living rats. Nanoscale 5, 8718–8723 (2013).
- ^ Jump up to:a b Kang J. H.; et al. (2014). “An extracorporeal blood-cleansing device for sepsis therapy”. Nat. Med 20: 1211–1216.doi:10.1038/nm.3640.
- Berry C. C.; Curtis A. S. G. (2003). “Functionalisation of magnetic nanoparticles for applications in biomedicine”. J. Phys. Appl. Phys.36: R198. doi:10.1088/0022-3727/36/13/203.
- Herrmann I. K.; et al. (2013). “Endotoxin Removal by Magnetic Separation-Based Blood Purification”. Adv. Healthc. Mater 2: 829–835.
- Lee J.-J.; et al. (2014). “Synthetic Ligand-Coated Magnetic Nanoparticles for Microfluidic Bacterial Separation from Blood”. Nano Lett.14: 1–5. doi:10.1021/nl3047305.
- Schumacher C. M.; et al. (2013). “Quantitative Recovery of Magnetic Nanoparticles from Flowing Blood: Trace Analysis and the Role of Magnetization”. Adv. Funct. Mater 23: 4888–4896. doi:10.1002/adfm.201300696.
- Yung C. W.; Fiering J.; Mueller A. J.; Ingber D. E. (2009). “Micromagnetic–microfluidic blood cleansing device”. Lab. Chip 9: 1171–7.doi:10.1039/b816986a.PMID 19370233.
- Herrmann, I. K., Grass, R. N. & Stark, W. J. High-strength metal nanomagnets for diagnostics and medicine: carbon shells allow long-term stability and reliable linker chemistry. Nanomed. 4, 787–798 (2009).
- Stacy Shepherd,“Harvard Engineers Invented an Artificial Spleen to Treat Sepsis”,Boston Magazine. Retrieved on 20 April 2015.
- Lalwani Gaurav; Henslee Allan M.; Farshid Behzad; Lin Liangjun; Kasper F. Kurtis, Yi-; Qin Xian; Mikos Antonios G.; Sitharaman Balaji; et al. (2013). “Two-dimensional nanostructure-reinforced biodegradable polymeric nanocomposites for bone tissue engineering”. Biomacromolecules 14 (3): 900–909. doi:10.1021/bm301995s.PMC 3601907. PMID 23405887.
- Lalwani, Gaurav (September 2013). “Tungsten disulfide nanotubes reinforced biodegradable polymers for bone tissue engineering”.Acta Biomaterialia 9 (9): 8365–8373. doi:10.1016/j.actbio.2013.05.018. PMC 3732565. PMID 23727293.
- Gobin AM; O’Neal DP; Watkins DM; Halas NJ; Drezek RA; West JL (2005). “Near infrared laser-tissue welding using nanoshells as an exogenous absorber”. Lasers Surg Med. 37 (2): 123–9. doi:10.1002/lsm.20206. PMID 16047329.
- http://www.nanowerk.com/spotlight/spotid=19573.php
- Nanomedicine, Volume IIA: Biocompatibility, by Robert A. Freitas Jr. 2003, ISBN 1-57059-700-6
- Freitas, Robert A., Jr.; Havukkala, Ilkka (2005). “Current Status of Nanomedicine and Medical Nanorobotics” (PDF). Journal of Computational and Theoretical Nanoscience 2(4): 1–25. doi:10.1166/jctn.2005.001.
- Nanofactory Collaboration
- Kurzweil, Ray (2005). The Singularity Is Near. New York City: Viking Press. ISBN 978-0-670-03384-3. OCLC 57201348.[page needed]
- Richard P. Feynman (December 1959). “There’s Plenty of Room at the Bottom”. Retrieved March 2010.
Further reading
///////////