BIA 10-2474
cas 1233855-46-3
3-(1-(cyclohexyl(methyl)carbamoyl)-1H-imidazol-4-yl)pyridine 1-oxide
1H-Imidazole-1-carboxamide, N-cyclohexyl-N-methyl-4-(1-oxido-3-pyridinyl)-
C16 H20 N4 O2, 300.36
| Bial-Portela & Ca. S.A. |

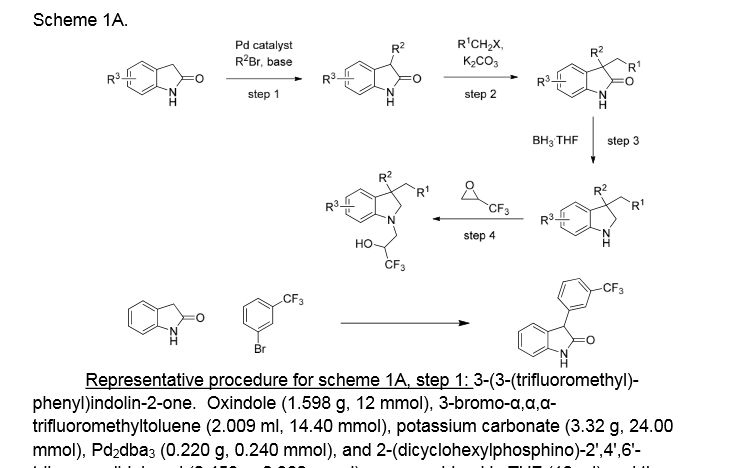
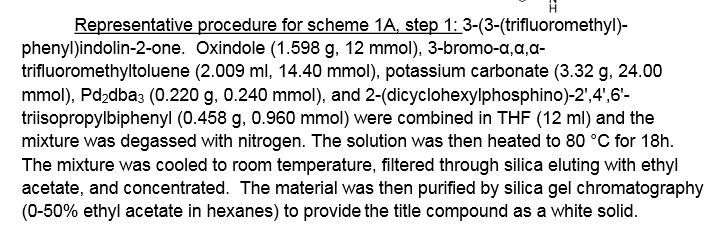
Synthesis
WO 2014017938
BIAL – PORTELA & Cª, S.A.Example 5. 3-(l-(cyclohexyl(methyl)carbamoyl-lfl-imidazol-4-yl)pyridine l-oxide (compound A)
C16H20N4O C16H20N4O2
MW 284,36 MW 300,36
To a solution of N-cyclohexyl-N-methyl-4-(pyridm-3-yl)-lH-imidazole-l-carboxamide in dichioromethane at 25°C was added peracetic acid (38%; the concentration is not critical, and may be varied) in a single portion. The reaction mixture was then maintained at 25°C for at least 20 h, whereupon the reaction was washed four times with water (in some embodiments, the water for the extraction step may be supplemented with a small amount (e.g. 1%) of acetic acid, which helps to promote product solubility in the DCM). The dichioromethane solution was then filtered prior to diluting with 2-propanol. Dichioromethane (50%) was then distilled off under atmospheric pressure, whereupon, 2-propanol was charged at the same rate as the distillate was collected. The distillation was continued until >90% of the dichioromethane was collected. The resulting suspension was then cooled to 20°C and aged for at least 30 min. prior to cooling to 0°C and aging for a further 60 min. The reaction mixture was then filtered and the product washed with additional 2-propanol, before drying at 50°C under vacuum to afford the title compound as an off-white crystalline solid.
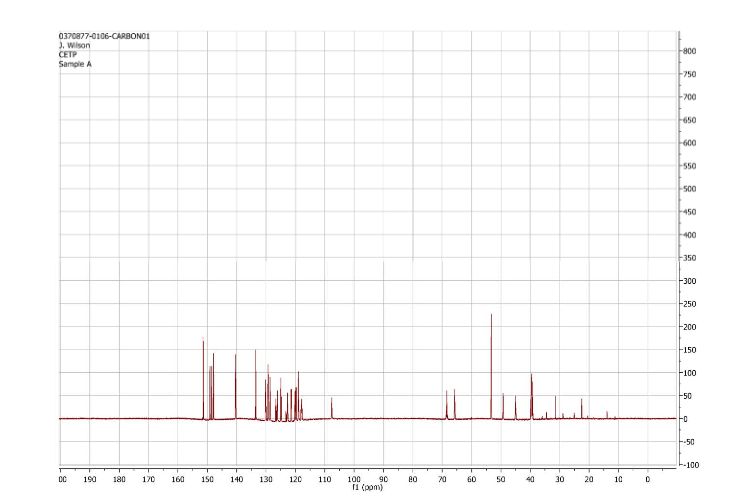
The purity of the product was ascertained by HPLC, with identity confirmable by NMR. The yield was consistently >80% in several production runs.
PATENT
WO 2012015324Example 1. Preparation of N-cyclohexyl-N-methyl-4-(pyridin-3yl)-lH-imidazole-l-carboxamide
C8H7N3 C15H1 1N302 C16H20N4O
MW 145,16 MW 265,27 MW 284,36
To a suspension of 3-(l/ -imidazol-4-yl)pyridine in tetrahydrofuran (THF) containing pyridine at 25°C was slowly added a solution of phenyl chloroformate in THF over 60 to 90 min. The resulting fine white suspension was then maintained at 25°C for at least 60 min. before the addition of N-methyl- -cyclohexylamine in a single portion, causing the suspension to thin and become yellow in colour. The reaction mixture was then stirred for 90 min. before filtering and washing the filter cake with additional THF. The mother liquors were then maintained at 25°C for at least 18 h, whereupon 65% of the volume of THF was distilled off under atmospheric pressure. The resulting solution was then diluted with 2-propanol and maintained at > 50°C for 10 min. prior to cooling down to 20°C. The resulting suspension was aged at 20°C for 15 min. prior to cooling to 0°C and aging for a further 60 min. The reaction mixture was then filtered and the product was washed with additional 2-propanol, before drying at 50°C under vacuum to afford the title compound as an off-white crystalline solid.
The purity of the product was ascertained by HPLC, with identity confirmable by NMR. The yield was consistently around 50% in several production runs.
Example 2. 3-(l-(cyclohexyl(methyl)carbamoyl-l//-imidazol-4-yl)pyridine 1 -oxide (compound A)
C16H20N4O Ci6H2oN402
MW 284,36 MW 300,36
To a solution of N-cyclohexyl-N-methyl-4-(pyridin-3-yl)-lH-imidazole-l-carboxamide in dichloromethane at 25°C was added peracetic acid (38%; the concentration is not critical, and may be varied) in a single portion. The reaction mixture was then maintained at 25°C for at least 20 h, whereupon the reaction was washed four times with water. The dichloromethane solution was then filtered prior to diluting with 2-propanol. Dichloromethane (50%) was then distilled off under atmospheric pressure, whereupon, 2-propanol was charged at the same rate as the distillate was collected. The distillation was continued until >90% of the dichloromethane was collected. The resulting suspension was then cooled to 20°C and aged for at least 30 min. prior to cooling to 0°C and aging for a further 60 min. The reaction mixture was then filtered and the product washed with additional 2-propanol, before drying at 50°C under vacuum to afford the title compound as an off-white crystalline solid.
The purity of the product was ascertained by HPLC, with identity confirmable by NMR. The yield was consistently >80% in several production runs. It will be appreciated that this gives an overall yield of compound A many times greater than that achieved in the prior art.
In a further run of this synthesis, in a 2L reactor to a mixture of N-cyclohexyl-N-methyl-4-(pyridin-3-yl)-l H- imidazole-l-carboxamide (90 g, 317 mmol) and dichloromethane (1350 ml) was added peracetic acid (84 ml, 475 mmol). The reaction mixture was stirred at 25°C. Completion of the reaction was monitored by HPLC for the disappearance of N-cyclohexyl-N-methyl-4-(pyridin-3-yl)-lH- imidazole- 1-carboxamide. After reaction completion a solution of sodium metabisulfite (60.2 g, 317 mmol) in water (270ml) was added to the reaction mixture maintaining the temperature below 30°C. After phase separation the organic phase was washed with water. After phase separation the organic phase was concentrated at atmospheric pressure until 5 vol. Then solvent was swapped to isopropanol (1350 ml) and the suspension was cooled to 0°C during 4 hours and stirred at that temperature for 1 hour. The resulting solid was collected by filtration and was rinsed with water (270 ml) and isopropanol (270 ml) to afford a white crystalline solid in 84.8g (89%).
PATENT
WO 2010074588
Preparation of compound 362 a) N-cyclohexyl-N-methyl-4-(pyridin-3-yl)- 1 H-imidazole- 1 -carboxamide
To a stirred suspension of 3-( 1 H-imidazol-4-yl)pyridine dihydrochloride (1.745 g, 8 mmol) in a mixture of tetrahydrofuran (29 mL) and DMF (2.90 mL) was added potassium 2-methylpropan-2-olate (1.795 g, 16.0 mmol) and the mixture was refluxed for 30 minutes. The resulting brown suspension was cooled to room temperature and treated with pyridine (0.979 mL, 12 mmol) and N,N-dimethylpyridin-4-amine (0.098 g, 0.8 mmol), followed by the addition of cyclohexyl(methyl)carbamic chloride (1.476 g, 8.4 mmol). The reaction was heated to 90 0C overnight, whereupon the mixture was diluted with water and extracted with ethyl acetate. The organic phase was dried (MgSO^) and filtered. After evaporation, the crude product was chromatographed over silica gel using a dichloromethane/methanol (9:1) mixture. Homogenous fractions were pooled and evaporated to leave a white powder, (160 mg, 7 %).
b) 3-( 1 -(cyclohexyl(methyl)carbamoyl)- 1 H-imidazol-4-yl)pyridine 1 -oxide
To a stirred solution of N-cyclohexyl-N-methyl-4-(pyridin-3-yl)-l H-imidazole- 1 -carboxamide (90 mg, 0.317 mmol) in chloroform (5 mL) was added 3-chlorobenzoρeroxoic acid (149 mg, 0.475 mmol) in one portion. The reaction was allowed to stir at room temperature for 20 h. TLC showed the reaction to be complete and the mixture was evaporated to dryness. The residue was triturated with ether and the resulting white crystals were filtered off and dried in air. Recrystallisation from hot isopropanol gave a white powder (46 mg, 46 %).
Structure and action
French newspaper Le Figaro has obtained Bial study protocol documents listing the the chemical name of BIA-10-2474 as 3-(1-(cyclohexyl(methyl)carbamoyl)-1H-imidazol-4-yl)pyridine 1-oxide.[8] A Bial news release described BIA-10-2474 as “a long-acting inhibitor of FAAH”.[9]Fatty acid amide hydrolase (FAAH) is an enzyme which degrades endocannabinoid neurotransmitters like anandamide,[10] which relieves pain and can affect eating and sleep patterns.[11][12] FAAH inhibitors have been proposed for a range of nervous-system disorders including anxiety, alcoholism, pain and nausea.
The Portuguese pharmaceutical company Bial holds several patents on FAAH enzyme inhibitors.[12][13][14][15]
No details of the preclinical testing of this molecule have been made public by the manufacturer Bial. However, the French newspaper Le Figaro has obtained and published an apparently legitimate copy of the full clinical trial protocol (BIA-102474-101).[8] The protocol presents a summary of what appears to be a full package of pharmacodynamic, pharmacokinetic and toxicological studies that might be expected to support a first-in-man study, including safety pharmacology studies in two species (rat, dog) and repeated dose toxicity studies in four species (13 week sub-chronic studies in mouse, rat, dog and monkey). The summary presented however includes no assessment of the relevance of the animal species selected for study (that is, in terms of physiological and genetic similarities with humans and the mechanism of action of the study drug).
Of note, few adverse events were observed in any of the studies, with the 13-week oral No Observed Adverse Effect Level (NOAEL) varying between 10 mg/kg/day in mice to 75 mg/kg/day in monkeys. The authors suggest that these were the maximum doses tested in these studies, though it is not clear. The authors also report no effects of significance in the animal models used for the CNS safety pharmacology studies, which studied a dose of up to 300 mg/kg/day.[8]
Notably absent from the protocol are calculations of receptor occupancy; predictions of in vivo ligand binding saturation levels; measures of target affinity; or assessment of the molecule’s activity in non-target tissues or non-target binding interactions as suggested by the European guidance for Phase I studies,[16] assuming BIA 10-2474 could be considered ‘high risk’).[8]
The trial protocol makes no reference to chimpanzee studies (only monkeys) which contradicts a previous statement to the media in which the French Health Minister stated that the drug had been tested on animals including chimpanzees.[4][17] [18] Some experts had remarked that drug testing in chimpanzees was unlikely.[19]
These findings provide no explanation for the type and severity of events observed in Rennes. In describing the rationale for the starting dose, the authors conclude that:
No target organ was identified during toxicology studies and few adverse clinical findings were observed at the highest dose tested. For the single ascending dose part [of the clinical trial], a starting dose of 0.25 mg was judged to be safe for a first-in-human administration. [8]The protocol defines no starting dose for the multi-dose treatment groups, noting that this will be based on the outcome of the single dose portion of the trial (an approach known as adaptive trial design). The authors note that nonetheless, the starting dose will not exceed 33% of the maximum tolerated dose (MTD) identified in the single dose groups (or 33% of the maximum administered dose if the MTD is not reached).[8]
Death and serious adverse events during phase I clinical trial
In July 2015 Biotrial, a contract research organization, began testing the drug in a human phase one clinical trial for the manufacturer. The study was approved by French regulatory authority, the Agence Nationale de Sécurité du Médicament (ANSM), on June 26, 2015, and by the Brest regional ethics committee on July 3, 2015.[20] The trial commenced on July 9, 2015,[21] in the city of Rennes, and recruited 128 healthy volunteers, both men and women aged 18 to 55. According to French authorities, the study employed a three-stage design with 90 of the volunteers having received the drug during the first two stages of the trial, with no serious adverse events being reported .[17][20] Participants of the study were to receive €1,900 and, in turn, asked to stay at Biotrial’s facility for two weeks during which time they would take the drug for ten days and undergo tests.[22]In the third stage of the trial evaluating multiple doses, six male volunteers received doses by mouth, starting on 7 January 2016. The first volunteer was hospitalized at the Rennes University Hospital on January 10, became brain dead,[17][23][24][25] and died on January 17.[26] The other five men in the same dosage group were also hospitalized, in the period of January 10 through January 13[27] four of them suffering injuries including deep hemorrhagic and necrotic lesions seen on brain MRI.[7] The six men who were hospitalised were the group which received the highest dose.[26] A neurologist at the University of Rennes Hospital Center, Professor Pierre-Gilles Edan, stated in a press conference with the French Minister for Health, that 3 of the 4 men who were displaying neurological symptoms “already have a severe enough clinical picture to fear that even in the best situation there will be an irreversible handicap” and were being given corticosteroids to control the inflammation.[27] The sixth man from the group was not showing adverse effects but had been hospitalized for observation.[25][28][29] Biotrial stopped the experiment on January 11, 2016.[4]
No details of the trial have been made public by the manufacturer Bial. The study does not appear in searches of any of the key clinical trial registries, including EudraCT and ClinicalTrials.gov which would normally contain details of approved clinical studies.[30][31][32][33] The trial protocol published by Le Figaro provides extensive detail on what was planned for the study, but many details of the key multi-dose part are not included and were to have been finalised at the conclusion of the single-dose part of the trial.[8]
The French health minister Marisol Touraine called the event “an accident of exceptional gravity” and promised to investigate the matter.[4] On January 18 it was reported authorities were investigating if a manufacturing or transport error might be involved.[34]
Le Figaro posted a 96-page clinical study protocol for BIA 10-2474 that the French newspaper procured from an unnamed source.
According to the document, BIA 10-2474 is 3-(1-(cyclohexyl(methyl)carbamoyl)-1H-imidazol-4-yl)pyridine 1-oxide.
BIA 10-2474 “is designed to act as a long-active and reversible
inhibitor of brain and peripheral FAAH,” notes the protocol. The
compound “increases anandamide levels in the central nervous system and
in peripheral tissues.”
The clinical trial protocol also notes that the company tested BIA
10-2474 on mice, rats, dogs, and monkeys for effects on the heart,
kidneys, and gastrointestinal tract, among other pharmacological and
toxicological evaluations.


Six men in a Phase I clinical trial were admitted to
the University Hospital Center of Rennes, France, (shown here) because
of adverse reactions.Six men in a Phase I clinical trial were admitted
to the University Hospital Center of Rennes, France, (shown here)
because of adverse reactions.
Credit: Mathieu Pattier/SIPA/Newscom
One man is dead and five men were hospitalized after participating in a Phase I clinical trial in Rennes, France
The clinical trial, conducted by the company Biotrial on behalf of the Portuguese pharmaceutical firm Bial,
was evaluating a pain relief drug candidate called BIA 10-2474 that
inhibits fatty acid amide hydrolase (FAAH) enzymes. Blocking these
enzymes prevents them from breaking down cannabinoids in the brain, a
family of compounds that includes the euphoria-inducing neurotransmitter
anandamide and Δ9-tetrahydrocannabinol, the major psychoactive component of marijuana.
Phase I clinical trials are conducted to check a drug candidate’s
safety profile in healthy, paid volunteers. In this case, the drug
caused hemorrhagic and necrotic brain lesions in five out of six men in a
group who received the highest doses of the drug, said Gilles Edan, a
neurologist at the University Hospital Center of Rennes.


The most severely affected man was pronounced brain-dead after
hospitalization and then died on Jan. 17. Four men remain in the
hospital in stable condition. The only man in the high-dose group who
had no adverse symptoms has been released from the hospital.
Clinical trials are an essential part of the drug development process. In order to get life-improving and life-saving medicines to patients, they first have to go through an extensive series of tests. Even before a drug makes it to Phase 1 testing, where its safety, dosage amount, and side effects are tested in a small group of humans, it will undergo testing in animals. As a result, it is not common for a medicine undergoing clinical tests to have a very serious adverse effect on a human. This makes you wonder what happened to a group of patients involved in a clinical study in Rennes, France.
According to news reports, a drug undergoing testing in a French clinic has left one person dead, two others with what may be permanent brain damage, and and two others critically ill. The drug has thus far been unnamed, but it appears to have been produced by the Portuguese company Bial. The French health minister has stated the drug acted on natural receptors found in the body known as endocannibinoids, which regulate mood and appetite. It did not contain cannabis or anything derived from it, as was originally reported. All six trial participants were administered the doses simultaneously.
The trial was being performed at Biotrial, a French-based firm that was formed in 1989 and has conducted thousands of trials. A message on the company’s website stated that they are working with health authorities to understand the cause of the accident, while extending thoughts to the patients and their families. Bial has disclosed the drug was a FAAH (fatty acid amide hydrolase) inhibitor, which is an enzyme produced in the brain and elsewhere that breaks down neurotransmitters called endocannabinoids. Two scientists from the Nottingham Medical School who have worked with FAAH tried over the weekend to try and identify the drug by examining a list of drugs Bial currently has in its pipeline. They believe the culprit is one identified by the codename BIA 10-2474. That same codename appeared on a recruitment form that was given to a volunteer, which was published in a French newspaper. Little more is known about it, and there does not appear to be any entry for it in clinical trial registries.
The French health ministry is reporting the six patients were all in good health prior to taking the oral medicine, which was administered to 90 volunteers. The trial recruited 128 individuals, and the remaining participants received a placebo. Health minister Marisol Touraine, describing the situation as a very serious accident, noted the patients were taking part in a trial in Brittany, Rennes involving a medicine developed by a “European laboratory”, refusing to comment further until additional information became available. She has also asked the Inspector General of Social Affairs to lead an investigation into the circumstances around the trial, which has obviously been suspended. She notes the drug had been tested on animals, including chimpanzees. France’s National Agency for Medicine and Health Products Safety approved the trial on in June 2015.
One thing we do know is that the trial was a Phase 1 clinical study that included 90 healthy volunteers. Regulations that oversee all clinical trials in Europe do attempt to minimize the risk associated with trials, but there is always a risk involved with administering an unapproved medicine to humans. At this time the chief neuroscientist at the hospital where the patients are being treated has said there is no known antidote for the drug.
The drug, administered to men between the ages of 28 and 49, was intended to treat mood disorders such as anxiety. While the men were administered varying doses, the patients who are hospitalized were taking the drug “regularly”.

This of course led many to wonder about the future of trials, and whether the situation could happen again. The Duff Report, written in response to the TGN1412 trial, noted the medicine should have been tested in one person at a time. It also helped to put additional safety measures in place. The Medicines and Health Products Regulatory Agency (MHRA) now requires committees to look at pre-clinical data to determine the proper initial dose, and rules are in place to stop the trial if unintended reactions occur.
However, since patients can fall ill immediately after being administered a medication, certain risks will still exist.
The company that manufactured TGN1412, TeGenero Immuno Therapeutics, later went bankrupt. However the drug was later purchased by a Russian investor and renamed TABO8. TheraMAB, a Russian biotech company, then conducted a new trial of the drug in a much lower dose. A later Phase 2 study was started in patients with Rheumatoid Arthritis.
Other pharmaceutical companies, including Merck, Pfizer, Johnson & Johnson, Sanofi and Vernalis, have previously taken other FAAH inhibitors into clinical trials without experiencing such adverse events (e.g. respectively, MK-4409,[35][36] PF-04457845, JNJ-42165279,[37] SSR411298 and V158866.[38][39] Related enzyme inhibitor compounds such as URB-597 and LY-2183240 have been sold illicitly as designer drugs,[40][41]
all without reports of this type of toxicity emerging, so the mechanism
of the toxicity observed with BIA 10-2474 remains poorly understood.Clinical trials are an essential part of the drug development process. In order to get life-improving and life-saving medicines to patients, they first have to go through an extensive series of tests. Even before a drug makes it to Phase 1 testing, where its safety, dosage amount, and side effects are tested in a small group of humans, it will undergo testing in animals. As a result, it is not common for a medicine undergoing clinical tests to have a very serious adverse effect on a human. This makes you wonder what happened to a group of patients involved in a clinical study in Rennes, France.
According to news reports, a drug undergoing testing in a French clinic has left one person dead, two others with what may be permanent brain damage, and and two others critically ill. The drug has thus far been unnamed, but it appears to have been produced by the Portuguese company Bial. The French health minister has stated the drug acted on natural receptors found in the body known as endocannibinoids, which regulate mood and appetite. It did not contain cannabis or anything derived from it, as was originally reported. All six trial participants were administered the doses simultaneously.
The trial was being performed at Biotrial, a French-based firm that was formed in 1989 and has conducted thousands of trials. A message on the company’s website stated that they are working with health authorities to understand the cause of the accident, while extending thoughts to the patients and their families. Bial has disclosed the drug was a FAAH (fatty acid amide hydrolase) inhibitor, which is an enzyme produced in the brain and elsewhere that breaks down neurotransmitters called endocannabinoids. Two scientists from the Nottingham Medical School who have worked with FAAH tried over the weekend to try and identify the drug by examining a list of drugs Bial currently has in its pipeline. They believe the culprit is one identified by the codename BIA 10-2474. That same codename appeared on a recruitment form that was given to a volunteer, which was published in a French newspaper. Little more is known about it, and there does not appear to be any entry for it in clinical trial registries.
The French health ministry is reporting the six patients were all in good health prior to taking the oral medicine, which was administered to 90 volunteers. The trial recruited 128 individuals, and the remaining participants received a placebo. Health minister Marisol Touraine, describing the situation as a very serious accident, noted the patients were taking part in a trial in Brittany, Rennes involving a medicine developed by a “European laboratory”, refusing to comment further until additional information became available. She has also asked the Inspector General of Social Affairs to lead an investigation into the circumstances around the trial, which has obviously been suspended. She notes the drug had been tested on animals, including chimpanzees. France’s National Agency for Medicine and Health Products Safety approved the trial on in June 2015.
One thing we do know is that the trial was a Phase 1 clinical study that included 90 healthy volunteers. Regulations that oversee all clinical trials in Europe do attempt to minimize the risk associated with trials, but there is always a risk involved with administering an unapproved medicine to humans. At this time the chief neuroscientist at the hospital where the patients are being treated has said there is no known antidote for the drug.
The drug, administered to men between the ages of 28 and 49, was intended to treat mood disorders such as anxiety. While the men were administered varying doses, the patients who are hospitalized were taking the drug “regularly”.

Old 2006 case
While safety issues like this are rare, they are not unheard of. In 2006, a clinical trial in London left six men ill. All were taking part in a study testing a drug designed to fight auto-immune disease and leukemia. Within hours of taking the drug TGN1412, all experienced a serious reaction, were admitted to intensive care, and had to be treated for organ failure. Two became critically ill, with one eventually losing all of his fingers and toes. All were told they would have a higher risk of developing cancers or auto-immune diseases.This of course led many to wonder about the future of trials, and whether the situation could happen again. The Duff Report, written in response to the TGN1412 trial, noted the medicine should have been tested in one person at a time. It also helped to put additional safety measures in place. The Medicines and Health Products Regulatory Agency (MHRA) now requires committees to look at pre-clinical data to determine the proper initial dose, and rules are in place to stop the trial if unintended reactions occur.
However, since patients can fall ill immediately after being administered a medication, certain risks will still exist.
The company that manufactured TGN1412, TeGenero Immuno Therapeutics, later went bankrupt. However the drug was later purchased by a Russian investor and renamed TABO8. TheraMAB, a Russian biotech company, then conducted a new trial of the drug in a much lower dose. A later Phase 2 study was started in patients with Rheumatoid Arthritis.
Following the events in Rennes, Janssen announced that it was temporarily suspending dosing in two Phase II clinical trials with its own FAAH inhibitor JNJ-42165279, headlining the decision as “precautionary measure follows safety issue with different drug in class”. Janssen was emphatic that no serious adverse events had been reported in any of the clinical trials with JNJ-42165279 to date. The suspension is to remain in effect until more information is available about the BIA 10-2474 study.[42]
References
- 1 “BRIEF-Bial says firmly committed to ensure wellbeing of test participants”. Reuters. 15 January 2016.
- 2 “BIA 10-2474”. Biocentury.com. Retrieved 2016-01-17.
- 3 “BIA 102474”. Adisinsight/springer.com. Retrieved 2016-01-17.
- 4 Adamson B (January 15, 2016). “Botched Drug Trial Leaves 1 Brain Dead, 5 in Hospital”. ABC, AP. Retrieved January 16, 2016.
- 5 Angeline Benoit,Makiko Kitamura (15 January 2016). “France Ties Brain-Dead Person to Tests of Bial-Portela Drug”. Bloomberg.com.
- 6 “France/Monde – Essai thérapeutique : 90 personnes ont pris la molécule”. Ledauphine.com. Retrieved 2016-01-17.
- 7 Enserink, Martin (2016). “More Details Emerge on Fateful French Drug Trial” (online). Science (January 16). Retrieved 16 January 2016.
- 8 “Drame de Rennes : le protocole de l’essai clinique en accusation”. sante.lefigaro.fr. Retrieved 2016-01-21.
- 9 “News Release – Phase I Clinical Trial Rennes”. http://www.bial.com. Retrieved 2016-01-21.
- 10 Debora Mackenzie. “Six in hospital after French pain relief drug trial goes wrong”. New Scientist.
- 11 “The Discovery and Development of Inhibitors of Fatty Acid Amide Hydrolase (FAAH)”. PubMed Central.
- 12 “Patent WO2015012708A1 – Imidazolecarboxamides and their use as faah inhibitors – Google Patents”. Google.com. Retrieved 2016-01-17.
- 13 “Patent WO2015016729A1 – Urea compounds and their use as faah enzyme inhibitors”. Google.com. Retrieved 2016-01-17.
- 14 “PT2014000052 UREA COMPOUNDS AND THEIR USE AS FAAH ENZYME INHIBITORS”. Patentscope.wipo.int. Retrieved 2016-01-17.
- 15 WO application 2015016729, Laszlo Erno KISS, Rita GUSMÃO DE NORONHA, Carla Patrícia ROSA DA COSTA PEREIRA, Rui PINTO, “Urea compounds and their use as faah enzyme inhibitors”, published Feb 5, 2015, assigned to BIAL
- 16″Strategies to identify and mitigate risks for first-in-human clinical trials with investigational medicinal products (CHMP/SWP/28367/07)” (PDF). European Medicines Agency. 1 September 2007. Retrieved 22 January 2016.
- 17 “Accident grave dans le cadre d’un essai clinique – Intervention de Marisol Touraine à Rennes”. Ministère des Affaires Sociales, de la Santé et des Droits des Femmes, France. 15 January 2016.
- 18Barbara Casassus (23 January 2016). “France investigates drug trial disaster” (PDF). The Lancet 387 (10016): 326. doi:10.1016/S0140-6736(16)00154-9.
- 19
- “Expert reaction to French drug trial – reports of one patient dying and five others in hospital and of the Paris prosecutor’s office having opened an investigation into what happened”. Science Media Centre, London. 16 January 2016. Retrieved 21 January 2016.
- 20
- “La survenue d’effets graves ayant entraîné l’hospitalisation de 6 patients, dont un en état de mort cérébrale, a conduit à l’arrêt prématuré d’un essai clinique du laboratoire BIAL – Point d’information”. Agence Nationale de Sécurité du Médicament, France (ANSM). 15 January 2016.
- 21
- “Six hospitalized in Bial clinical trial in France”. BioWorld.com. Retrieved 2016-01-17.
- 22
- Enserink M (January 16, 2016). “More details emerge on fateful French drug trial”. Science Magazine. Retrieved January 18, 2016.
- 23
- “France clinical trial: 90 given drug, one man brain-dead”. BBC. January 15, 2016. Retrieved January 16, 2016.
- 24
- “Ce que l’on sait de l’accident survenu lors d’un essai clinique à Rennes”, Le Monde, 15 January 2016
- 25
- Blamont M (January 15, 2016). “French drug trial disaster leaves one brain dead, five injured”. Reuters. Retrieved January 16, 2016.
- 26
- Clarisse Lucas, AFP (January 17, 2016). “Man dies after being left brain-dead in French drug trial”. Yahoo. Retrieved January 17, 2016.
- 27
- “Accident “inédit” lors d’un essai clinique: un homme en état de mort cérébrale, cinq hospitalisés”. La Depeche. January 15, 2016. Retrieved January 18, 2016.
- 28
- “France clinical trial: ‘No known antidote’ to drug”. BBC News. 15 January 2016. Retrieved 18 January 2016.
- 29
- Enserink, Martin (2016). “What We Know So Far About the Clinical Trial Disaster in France” (online). Science (January 15). Retrieved 16 January 2016.
- 30
- “EU Clinical Trials Register”. European Medicines Agency. Retrieved 20 January 2016.
- 31
- “WHO International Clinical Trials Registry Platform”. World Health Organization. Retrieved 20 January 2016.
- 32
- “ANSM – Répertoire public des essais cliniques de médicaments”. Agence Nationale de Sécurité du Médicament et des Produits de Santé, France. Retrieved 20 January 2016.
- 33
- “ClinicalTrials.gov Registry”. U.S. National Institutes of Health. Retrieved 20 January 2016.
- 34
- “Drug trial volunteer dies as ‘manufacturing error’ theory investigated”. The Independent. January 18, 2016. Retrieved January 18, 2016.
- 35
- Chobanian; et al. (10 April 2014). “Discovery of MK-4409, a Novel Oxazole FAAH Inhibitor for the Treatment of Inflammatory and Neuropathic Pain”. ACS Med. Chem. Lett.
- 36
- Merck (15 October 2009). “Merck Pipeline, Oct 2009” (PDF). Merck.
- 37
- “Seven studies found for: jnj-42165279”. Clinicaltrials.gov. Retrieved 2016-01-19.
- 38
- “2 studies found for: V158866”. Clinicaltrials.gov. Retrieved 2016-01-19.
- 39
- Bisogno T, Maccarrone M. Latest advances in the discovery of fatty acid amide hydrolase inhibitors. Expert Opin Drug Discov. 2013 May;8(5):509-22. PMID 23488865 doi: 10.1517/17460441.2013.780021.
- 40
- Shanks KG, Behonick GS, Dahn T, Terrell A. Identification of novel third-generation synthetic cannabinoids in products by ultra-performance liquid chromatography and time-of-flight mass spectrometry. J Anal Toxicol. 2013 Oct;37(8):517-25. PMID 23946450 doi: 10.1093/jat/bkt062.
- 41
- Uchiyama N, Matsuda S, Kawamura M, Shimokawa Y, Kikura-Hanajiri R, Aritake K, Urade Y, Goda Y. Characterization of four new designer drugs, 5-chloro-NNEI, NNEI indazole analog, α-PHPP and α-POP, with 11 newly distributed designer drugs in illegal products. Forensic Sci Int. 2014 Oct;243:1-13. PMID 24769262 doi: 10.1016/j.forsciint.2014.03.013.
- “Janssen Research & Development, LLC Voluntarily Suspends Dosing in Phase 2 Clinical Trials of Experimental Treatment for Mood Disorders”. Janssen.com. 17 January 2016. Retrieved 21 January 2016.
External links
| WO2005073199A1 * | Jan 15, 2005 | Aug 11, 2005 | Aventis Pharma Gmbh | Indazole derivatives as inhibitors of hormone-sensitive lipases |
| WO2010074588A2 | Dec 23, 2009 | Jul 1, 2010 | BIAL – PORTELA & Cª, S.A. | Pharmaceutical compounds |
| WO2012015324A1 | Jul 28, 2011 | Feb 2, 2012 | Bial – Portela & Ca, S.A. | Process for the synthesis of substituted urea compounds |
| US4051252 * | Nov 24, 1975 | Sep 27, 1977 | Bayer Aktiengesellschaft | 3-aminoindazole-1 and 2-carboxylic acid derivatives |
| US4331678 * | Jan 14, 1980 | May 25, 1982 | Fbc Limited | Carbamoyl pyrazole compounds and their pesticidal application |
| US4973588 * | Feb 10, 1989 | Nov 27, 1990 | Mitsui Petrochemical Industries, Ltd. | Imidazole derivatives having anti-hypoxia properties |
| US5578627 * | Oct 27, 1993 | Nov 26, 1996 | Toyama Chemical Co., Ltd. | 1,2-benzoisoxazole derivative or its salt and brain-protecting agent comprising the same |
 |
|||||
| Systematic (IUPAC) name | |||||
|---|---|---|---|---|---|
|
3-(1-(cyclohexyl(methyl)carbamoyl)-1H-imidazol-4-yl)pyridine 1-oxide
|
|||||
| Clinical data | |||||
| Legal status |
|
||||
| Routes of administration |
Oral | ||||
| Identifiers | |||||
| PubChem | CID: 46831476 | ||||
| Chemical data | |||||
| Formula | C16H20N4O2
|
||||
C1C(CCCC1)N(C)C(=O)n2cc(nc2)c3ccc[n+](c3)O